How is Depression Treated?
How is Depression Treated?
Depression is one of the most treatable mental disorders. 80% to 90% percent of people with depression eventually respond well to treatment. Almost all patients get some relief from their symptoms.
Before diagnosis or treatment, a health professional should conduct a thorough clinical evaluation, including an interview and physical examination.
The assessment will identify specific symptoms and explore medical and family history and cultural and environmental factors, to arrive at a diagnosis and formulate a plan of action.
In some cases, blood tests may be done to ensure the depression is not caused by a medical condition such as a thyroid problem or vitamin deficiency (reversing the medical cause will reduce depression-like symptoms).
Medicine
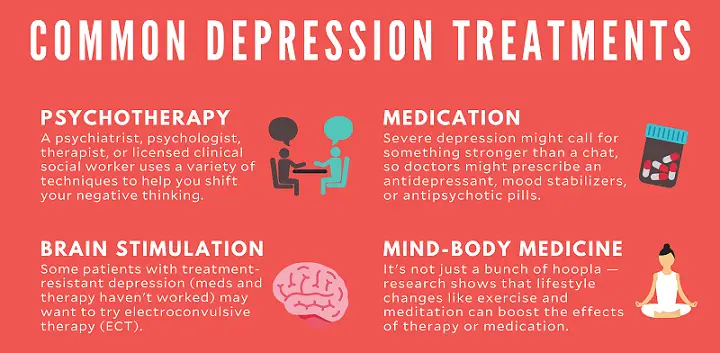
Brain chemistry may contribute to a person’s depression and may factor into their treatment. For this reason, antidepressants may be prescribed to help modify one’s brain chemistry. These drugs are not sedatives, “highs,” or tranquillizers. They are not habit-forming. Antidepressant drugs usually have no stimulating effect on people who do not experience depression.
Antidepressants may produce some improvement within the first week or two of use, but full benefits may not be seen for two to three months. If a patient feels little or no improvement after several weeks, their psychiatrist may change the dosage of the drug or add or replace another antidepressant.
Other psychotropic medications may be helpful in some situations. It is important to tell your doctor if a medicine does not seem to work or if you experience side effects.
Psychiatrists usually recommend that patients continue taking medication for six or more months, even after symptoms have improved. Long-term maintenance treatment may be suggested for some people at high risk to reduce the risk of future episodes.
Psychotherapy
Psychotherapy, or “talk therapy”, is sometimes used alone to treat mild depression; For moderate to severe depression, psychotherapy is often used along with antidepressant medications. Cognitive behavioural therapy (CBT) is effective in treating depression.
CBT is a form of treatment that currently focuses on problem-solving. CBT helps a person identify distorted/negative thinking to change thoughts and behaviours to respond to challenges more positively.
Psychotherapy may involve only the individual but may include others. For example, family or couples therapy can help address issues within these close relationships.
Group therapy brings people with similar illnesses together in a supportive environment and can help the participant learn how others cope with similar situations.
Depending on the severity of the depression, treatment may take a few weeks or longer. Significant improvement can be made in 10 to 15 sessions in many cases.
Electroconvulsive Therapy (ECT)
ECT is a medical treatment usually reserved for patients with severe depression who have not responded to other treatments. This involves a brief electrical stimulation of the brain while the patient is under anesthesia.
A patient typically receives ECT two to three times a week for a total of six to 12 treatments. A team of trained medical professionals, including a psychiatrist, an anesthesiologist and a nurse or physician assistant, usually manage it.
ECT has been used since the 1940s, and many years of research have led to major improvements and recognition of its effectiveness as a mainstream rather than “last resort” treatment.
Self-Help and Coping
There are many things people can do to help ease the symptoms of depression. For many people, regular exercise helps create positive feelings and improves mood. Getting enough quality sleep regularly, eating a healthy diet, and avoiding alcohol (a depressant) may also help reduce symptoms of depression.
Depression is a real illness, and help is available. With proper diagnosis and treatment, most people with depression will overcome it. If you’re experiencing symptoms of depression, the first step is to see your family doctor or a psychiatrist. Talk about your concerns and request an in-depth evaluation. This is just the beginning of meeting your mental health needs.
Related Terms:-
- Peripartum depression (first postpartum depression)
- Seasonal depression (also called seasonal affective disorder)
- bipolar disorder
- Persistent depressive disorder (previously dysthymia) (details below)
- premenstrual dysphoric disorder (details below)
- Disruptive Mood Disorder Disorder (details below)
Premenstrual Dysphoric Disorder (PMDD)
PMDD was added to the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) in 2013. A woman with PMDD has severe symptoms of depression, irritability, and tension about a week before her period starts.
Common symptoms include mood swings, irritability or anger, depressed mood, and marked anxiety or tension.
Other symptoms may include loss of interest in normal activities, difficulty concentrating, lack of energy or easy fatigue, changes in appetite with cravings for specific foods, trouble sleeping or sleeping too much, or feeling overwhelmed or out of control.
Physical symptoms may include breast tenderness or swelling, joint or muscle pain, “bloating”, or weight gain. Emotion may be involved.
These symptoms start one week to 10 days before the start of menstruation and improve or stop around the beginning. Symptoms cause significant distress and problems with routine functioning or social interactions.
To be diagnosed with PMDD, symptoms must have occurred in most menstrual cycles during the past year and adversely affected work or social functioning. Premenstrual dysphoric disorder is estimated to affect between 1.8% and 5.8% of menstruating women yearly.
PMDD can be treated with antidepressants, birth control pills, or nutritional supplements. Diet and lifestyle changes, such as reducing caffeine and alcohol, getting enough sleep and exercise, and practising relaxation techniques, can help.
Premenstrual syndrome (PMS) is similar to PMDD in that symptoms occur seven to 10 days before a woman’s period starts. However, PMS tends to involve fewer and less severe symptoms than PMDD.
Disruptive Mood Dysregulation Disorder
Disruptive mood dysregulation disorder is a condition that occurs in children and young people between the ages of 6 and 18. It involves chronic and severe irritability that results in harsh and frequent outbursts of anger.
Outbursts of anger can be verbal or include behaviours such as physical aggression towards people or property. These outbreaks are significantly disproportionate to the situation and are not commensurate with the child’s developmental age.
They must frequently occur (an average of three or more times per week) and usually in response to frustration. Between outbursts, the child’s mood is persistently irritable or angry most of the day, almost every day. This mood is noticeable in others, such as parents, teachers, and peers.
Mood dysregulation disorder is much more common in men than in women. It may occur with other diseases, including major depressive disorder, attention-deficit/hyperactivity disorder, anxiety, and conduct disorder.
For a disruptive mood dysregulation disorder diagnosis, symptoms must be present in at least two settings (e.g. at home, at school, with peers) for at least one year, and the condition must have started before age 10.
Disruptive mood dysregulation disorder can significantly impact a child’s ability to function and substantially affect the family. Chronic irritability and temper outbursts can disrupt family life, make it difficult for the child/young person to make or keep friendships, and cause difficulties at school.
Treatment usually involves psychotherapy (cognitive behavioural therapy) and medications.
Persistent Depressive Disorder
A person with persistent depressive disorder (previously referred to as dysthymic disorder) has a depressed mood for most days, most days, for at least two years. Attitude may be irritable or depressed in children and adolescents and must persist for at least one year.
In addition to a depressed mood, symptoms include:
- loss of appetite or overeating
- insomnia or hypersomnia
- low energy or fatigue
- low self-esteem
- poor concentration or difficulty making decisions
- sense of hopelessness
The persistent depressive disorder often begins in childhood, adolescence, or early adulthood and affects an estimated 0.5% of adults in the United States each year. Individuals with a persistent depressive disorder often describe their mood as sad or “down in the dumps”. Because these symptoms have become part of the person’s day-to-day experience, they may not seek help simply by assuming, “I’ve always been like this.”
Symptoms cause significant distress or difficulty with work, social activities, or other important areas of functioning. While the impact of the persistent depressive disorder on work, relationships, and daily life can vary widely, its impact can be as great as or greater than that of major depressive disorder.
A major depressive episode may precede the onset of persistent depressive disorder but may also occur during (and be superimposed on) a previous diagnosis of persistent depressive disorder.
Treating sleep problems may help prevent depression.
Sleep problems and depression are closely related and have a bidirectional relationship. Depression can make sleep problems worse, and disturbed sleep can cause depression symptoms to get worse.
Insomnia is common
Insomnia, the most common sleep disorder, involves problems falling asleep or staying asleep. About one-third of adults report some insomnia symptoms, 10–15% report problems with daytime functioning, and 6–10% have symptoms severe enough to meet the criteria for an insomnia disorder.
An estimated 40–50% of people with insomnia also have another mental illness. Insomnia is the most common type of sleep problem in people with depression – occurring in about 80 to 90% of people with depression. The authors note that it is rare for a person with major depression not to experience some sleep problems.
Insomnia significantly increases the risk of depression.
Insomnia is a well-understood risk factor for depression. Research has found that having insomnia doubles a person’s chances of developing depression. This risk is similar to the risk associated with having a close relative with major depressive disorder.
Emerging technologies make sleep tracking more accessible.
Emerging wearable technologies to track sleep and sleep problems at home, suggests Plante, “offer great potential to advance clinical care and research.”
They can be used early in treatment to help personalize treatments. However, he cautions that these new techniques need further testing and validation for sleep assessment and treatment, especially among people with depression.
There are effective treatments available for insomnia.
Insomnia is usually treated with either psychotherapy or medication. Specifically, cognitive-behavioural therapy for insomnia (CBT-I) is a highly effective non-drug treatment and “is generally considered a first-line therapeutic strategy,” notes Plante.
In recent years, Internet-based or digital CBT-I has generally shown benefits for insomnia and depressive symptoms in large-scale studies.
Lifestyle and complementary approaches may also help address insomnia, such as relaxation techniques, meditation, yoga, melatonin supplements, and daily exercise before bedtime, sticking to a sleep schedule.
Herbs and dietary supplements are not effective for insomnia. (If you are taking alternative medicines or supplements, tell your healthcare provider about them.)
Advances in understanding and treating sleep issues promise to help treat and prevent depression. Plante specifically suggests: “From a public health perspective, it may be possible to target insomnia in treating depression.
More important and useful may be the earlier time to the onset of a depressive episode. The development of effective Internet-based CBT-I therapies makes this increasingly possible. Furthermore, because sleep is closely linked to many mental health disorders, These advances could potentially be used to help treat other mental health conditions.











